RGUHS Nat. J. Pub. Heal. Sci Vol: 15 Issue: 4 eISSN: pISSN
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Lakshmi Priya Lalitha, Assistant Professor, Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India.
2Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India
3Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India
4Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India
5Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India
6Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India
*Corresponding Author:
Dr. Lakshmi Priya Lalitha, Assistant Professor, Department of Neurology, M S Ramaiah Medical College, Gokula, Bangalore, Karnataka, India., Email: lalithapriya.68@gmail.com
Abstract
Transverse myelitis is a rare neurological manifestation of antiphospholipid antibody syndrome. Most previously reported cases present with an acute or subacute onset, whereas chronic presentations are extremely rare and pose a significant diagnostic challenge. We report a case of middle-aged female with a prior history of unprovoked deep vein thrombosis of the right lower limb, who presented with gradually progressive symptoms suggestive of non-compressive cervical myelopathy. Blood investigations revealed a triple-positive antiphospholipid antibodies profile, with no clinical or immunological evidence of the commonly associated systemic lupus erythematosus (SLE). She was treated with high-dose steroids and mycophenolate mofetil, and demonstrated mild to moderate clinical improvement after six months of follow-up.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Antiphospholipid syndrome (APS) is an autoimmune condition characterized by one or more of the following: (a) vascular thrombotic events (arterial, venous or small vessel thrombosis in one or more organs); (b) pregnancy morbidity (embryonic loss <10 weeks, fatal loss, prem-ature birth); (c) One or more positive anti-phospholipid antibodies (serum or plasma anticardiolipin IgG/M, serum or plasma beta2-glycoprotein I IgG/M, lupus anticoagulant in plasma) on two or more occasions at least 12 weeks apart, according to the revised Sydney consensus criteria for diagnosis.1 APS may occur in association with other systemic inflammatory rheumatic diseases, most commonly systemic lupus erythematosus (secondary APS) or without its association (primary APS or Hughes syndrome). Clinical manifestations not included in the diagnostic criteria, but known to be asso-ciated with APS are termed “non-criteria features”. These features often contribute to diagnostic uncertainty and may include autoimmune cytopenias, nephropathy, Libman-Sacks endocarditis, livedo reticularis, and various neurological manifestations like young stroke, epilepsy, headache, movement disorders, neuropsychiatric manifestations, multiple sclerosis-like symptoms, and transverse myelitis.2
Among the neurological presentations, migraine and cognitive dysfunction are often reported, while others are extremely rare. In this context, we present a rare case of non-compressive cervical myelopathy secondary to antiphospholipid antibody syndrome.
Case Presentation
A 43-year-old female presented with a one-year history of gradually progressive, asymmetrical onset weakness of both upper limbs, initially manifesting as difficulty gripping objects, followed by difficulty lifting her hand above shoulder level. She denied any sensory symptoms, bowel and bladder disturbances. She had a prior history of right lower limb deep venous sinus thrombosis two years prior, and was started on oral anticoagulation that she discontinued on her own after one year. The etiological evaluation at that time had been suboptimal. On general examination, the patient was conscious, oriented, and moderately built and nourished, without any cutaneous markers suggestive of connective tissue disease. Neurological examination showed normal higher mental functions and intact cranial nerves. There was spasticity of all four limbs (more pronounced in the upper limbs), wasting of the small muscles of both hands, and proximal power in both upper limbs graded at 3-4/5, with a poor bilateral hand grip (40-50%). Lower limb power was greater than 4/5 bilaterally. Deep tendon reflexes were exaggerated in both upper and lower limbs. Hoffman’s sign was positive in both the upper limbs, and plantar responses were extensor bilaterally. Sensory examination findings were inconsistent. No fasciculations, extrapyramidal signs, or cerebellar deficits were noted. Clinical possibilities considered were: (a) Anterior horn cell disease, given the asymmetrical onset of motor weakness and atrophy with preserved bowel and function, though the absence of fasciculations and inconsistent sensory findings were atypical; (b) Cervical myelopathy, suggested by the presence of pyramidal signs in both lower limbs.
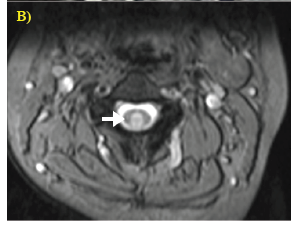
Her routine blood investigations were within normal limits. Based on the clinical localization, an MRI of the cervical spine with whole spine screening was performed, which showed a T2 hyperintense lesion extending from the C2-C3 level without any contrast enhancement (Figure 1). MRI brain screening was normal. Electroneuromyography (ENMG) performed to evaluate for a possible anterior horn cell disease, showed no evidence of active denervation. Blood investigations were planned to rule out common causes of non-compressive myelopathy. Serum vitamin B12 levels, thyroid function tests, and serum VDRL (Venereal Disease Research Laboratory) were non-contributory. Cerebrospinal fluid (CSF) analysis revealed 13 cells/mm3 (100% lymphocytes), mildly elevated proteins (48 mg/ dL), and normal glucose (67 mg/dL). CSF oligoclonal bands were negative. Serum Neuromyelitis Optica (NMO) and Myelin Oligodendrocyte Glycoprotein (MOG) were negative. Serum ANA (antinuclear antibodies) by immunofluorescence showed strong positivity (3+, homogenous nuclear pattern), while her ANA profile was negative. Plasma anticardiolipin IgG was positive, anti-beta 2-glycoprotein 1 - IgG was strongly positive, and lupus anticoagulant was detected. Antibody positivity was reconfirmed after 12 weeks.
Thus, she fulfilled both the clinical and laboratory criteria for anti-phospholipid antibody syndrome according to the revised Sydney criteria. She neither had cutaneous manifestations nor laboratory evidence of systemic lupus erythematosus (SLE), which is commonly associated with APS. She was treated with high dose IV methylprednisolone (1000 mg) for five days, followed by oral steroids at 1 mg/kg/day, which were gradually tapered during follow-up. After discussing available treatment options, mycophenolate mofetil (500 mg BD) was initiated. She also underwent limb physiotherapy and gait training under the supervision of a trained physiotherapist. At the time of discharge, there was no significant improvement. However, after six months of follow-up, she demonstrated mild improvement in upper limb power and was able to feed herself, though with mild clumsiness (bilateral upper limb proximal power 4/5, distal hand grip 60% bilaterally). There were no new neurological deficits compared to the initial assessment. She remained ambulant without any assistance, and her overall functional status had not deteriorated. Anticoagulation with a vitamin K antagonist (target INR 2-3) was continued in view of her prior lower limb deep venous thrombosis, and she is being regularly followed up.
Discussion
We report a case of a middle-aged female with chronic, progressively worsening symptoms of cervical myelopathy over one year, in the context of a previously unevaluated deep venous thrombosis. This background helped us to attribute the etiological possibility with certainty. The patient demonstrated significant clinical improvement following treatment with steroids and mycophenolate mofetil over a six-month follow-up period. The estimated prevalence of transverse myelitis among patients with antiphospholipid syndrome is <1%.3 Acute neurological presentation can be attributed to the proth-rombotic state of APS, leading to ischemic lesions.1 In addition, there is a recent evidence of inflammatory cascade, in which APS antibodies induce endothelial dysfunction, disrupt blood brain barrier break-down, and bind directly to CNS antigens, resulting in non-thrombotic pathology.4 Apart from transverse myelitis, other neurological manifestations postulated to occur from similar non-thrombotic mechanisms include, headache, seizures, multiple sclerosis-like disease, cognitive impairment, auto-nomic dysfunction, neuropsychiatric manifestations, and peripheral neuropathy.5
The clinical features of prior reported cases are summarized in Table 1. Most patients with antiphospho-lipid syndrome associated transverse myelitis have demon-strated an acute to subacute onset, in contrast to our case and one additional report by Berek et al. (2020).6 The age at presentation has ranged from 19 to 74 years, with an approximately equal distribution between the sexes. In our patient, as well as in the case reported by Berek et al., all three anti-phospholipid associated antibodies (anticardiolipin IgG or IgM, beta2-glycoprotein I IgG/M, lupus anticoagulant - called high-risk APS profile, EULAR recommendations 2019) were found to be persistently elevated, which was not observed in other reported cases, where only one or two antibodies were positive.7 This finding prompts us to hypothesize that a chronic presentation of transverse myelitis may be more likely in patients with triple antibody positivity.
Earlier diagnosis and prompt initiation of treatment are associated with favourable outcomes, as evidenced in previously reported cases. Significant clinical improvement was observed in patients who received steroids within 1-2 weeks of symptom onset, whereas those in whom treatment was delayed beyond 3-4 months showed minimal or no improvement. In contrast, patients with a chronic presentation, such as ours, tend to exhibit delayed clinical improvement, though the extent is uncertain. In this patient with definite APS syndrome, and a history of unprovoked thrombotic events, lifelong anticoagulation with a vitamin K antagonist targeting an INR of 2-3 was initiated, in accordance with the recent European Alliance of Associations for Rheumatology (EULAR) recommendations for APS management.7 Rivaroxaban or direct acting oral anticoagulants are not recommended in patients with high risk triple positivity given the current evidence indicating their poor efficacy.7,8 Should the patient experience recurrent thrombotic events, EULAR guidelines recommend increasing the target INR to 3-4 with close monitoring of INR or shift to low molecular weight heparin in combination with low-dose aspirin.7 The choice of immunosuppressive agents is based on case reports, with cyclophosphamide and azathioprine showing beneficial outcomes, as shown in Table 1. Additionally, two reports have described the use of plasmapheresis, both demonstrating favourable clinical responses.
Catastrophic anti-phospholipid syndrome is a life-threatening condition characterized by multi-organ thrombosis, usually precipitated by infection, surgical procedures, or discontinuation of anticoagulation. Recent clinical practice guidelines recommend combination therapy with glucocorticoids, heparin and either intravenous immunoglobulin (IVIG) or plasma exchange, along with concurrent management of precipitating factors.10 In refractory cases, B-cell depletion (rituximab) and complement inhibition (eculizumab) therapies have shown benefit in a few case reports.10 This case demonstrates a rare chronic form of transverse myelitis in triple-positive antiphospholipid antibody syndrome without systemic lupus erythematosus. The outcome in such patients is difficult to predict due to the rarity of this presentation. However, early diagnosis and prompt initiation of high-dose steroids along with immunosuppressive agents are considered ideal for optimal outcomes. Continued anticoagulation is essential to prevent thrombotic complications in these high-risk patients.
Conflict of Interest
Nil
Supporting File
References
1. Miyakis S, Lockshin MD, Atsumi T, et al. Intern-ational consensus statement on an update of the classification criteria for definite anti-phospholipid syndrome (APS). J Thromb Haemost 2006;4(2): 295-306.
2. Leal Rato M, Bandeira M, Romão VC, et al. Neurologic manifestations of the anti-phospholipid syndrome-an update. Curr Neurol Neurosci Rep 2021;21(8):41.
3. Ruiz-Irastorza G, Crowther M, Branch W, et al. Antiphos pholipid syndrome. Lancet 2010;376(9751):1498-509.
4. Fleetwood T, Cantello R, Comi C. Antiphospholipid syndrome and the neurologist: from pathogenesis to therapy. Front Neurol 2018;9:1001.
5. Sanna G, D'Cruz D, Cuadrado MJ. Cerebral mani-festations in the antiphospholipid (Hughes) syn-drome. Rheum Dis Clin North Am 2006;32(3): 465-90.
6. Berek K, Fava E, Zinganell A, et al. Transverse myelitis as a rare presentation of antiphospholipid-antibody-associated disorders. Mult Scler Relat Disord 2020;45:102405.
7. Tektonidou MG, Andreoli L, Limper M, et al. EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis 2019;78(10):1296-304.
8. Pengo V, Denas G, Zoppellaro G, et al. Rivaroxaban vs warfarin in high-risk patients with antiphospholipid syndrome. Blood 2018;132(13):1365-71.
9. Nomura Y, Takatsu R, Fujisawa K, et al. A case of transverse myelitis caused by primary antipho-spholipid antibody syndrome. Rinsho Shinkeigaku 1999;39(9):976-8.
10. Legault K, Schunemann H, Hillis C, et al. McMas-ter RARE‐Bestpractices clinical practice guideline on diagnosis and management of the catastrophic antiphospholipid syndrome. J Thromb Haemost 2018;16(8):1656-64.
11. Sherer Y, Hassin S, Shoenfeld Y, et al. Transverse myelitis in patients with antiphospholipid antibo-dies the importance of early diagnosis and treatment. Clin Rheumatol 2002;21(3):207-10.
12. Lee DM, Jeon HS, Yoo WH. Transverse myelitis in a patient with primary antiphospholipid syndrome. Yonsei Med J 2003;44(2):323-7.