RGUHS Nat. J. Pub. Heal. Sci Vol: 15 Issue: 4 eISSN: pISSN
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Kalpana Daga, Final Year Postgraduate, Department of ENT, KMCRI, Hubballi, Karnataka, India.
2Department of ENT, Karnataka Medical College and Research Institute, Hubballi, Karnataka, India.
3Department of ENT, Karnataka Medical College and Research Institute, Hubballi, Karnataka, India.
*Corresponding Author:
Dr. Kalpana Daga, Final Year Postgraduate, Department of ENT, KMCRI, Hubballi, Karnataka, India., Email: dr.kalpanadaga.ent@gmail.com
Abstract
Hyalohyphomycosis is an opportunistic infection of the subcutaneous tissue caused by hyaline fungi (Hyphomycetes) that form septate hyphae within tissue. Immunocompromised states and tropical climates are the main predisposing factors. Rhino-orbital hyalohyphomycosis involving the paranasal sinuses and orbit in an immunocompetent host is a very rare presentation. We report the case of a 27-year-old male crop surveyor who presented with left-sided proptosis and double vision. Based on clinical evaluation, and imaging studies-contrast enhanced tomography (CECT) and magnetic resonance imaging (MRI) of the paranasal sinuses and orbits - the findings were suggestive of an orbital pseudotumour or fungal mass such as mucormycosis. The patient underwent endoscopic sinus surgery with excision of the orbital mass via Denker's approach under general anaesthesia. Histopathological examination confirmed the diagnosis of hyalohyphomycosis. Postoperatively, the patient was treated with anti-fungal medication (Itraconazole) and advised regular nasal saline irrigation. Although rare in immunocompetent individuals, rhino-orbital hyalohyphomycosis should be considered among the differential diagnoses for unilateral intraorbital mass or proptosis.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Hyalohyphomycosis refers to infections caused by hya-line fungi (Hyphomycetes) that form septate hyphae in tissue. These hyphae are clear, light-coloured, or colo urless, and septate, each representing a fungal cell. In humans, most hyalohyphomycoses are opportunistic infections. The primary causative agents include Fusarium, Pseudallescheria, Scedosporium, Paecilomyces, Purpureocillium, Acremonium, Glio-mastix, Sarocladium, Penicillium, Scopulariopsis, Beauveria, and Trich oderma. Among these, Scedos-porium and Scopulariopsis are commonly associated with hyalohyphomycosis. Although Asper-gillus also produces hyaline septate hyphae and is considered a hyalohyphomycete, infections caused by this genus are typically termed as aspergillosis.1
Fungal species causing hyalohyphomycosis are widely distributed in nature and can be found in wood, decaying plant matter, and various types of soil. These fungi can infect individuals of any age or gender, especially those who are immunocompromised.
Clinically, hyalohyphomycosis is categorized into three forms: superficial, subcutaneous, and systemic. Superficial hyalohyphomycosis occurs more frequently among premature newborns, fishermen, rural labourers, and patients with severe onychomycosis or dermatomycosis.
Subcutaneous hyalohyphomycosis typically results from traumatic inoculation and manifests as tumour-like growths, cysts, or abscesses. Systemic infections are un-common but often severe, affecting immuno-suppressed individuals and potentially leading to fatal outcomes.2 We report a case of submucoperiosteal hyalohyphomycosis involving the rhino-orbital region in an immunocompetent host, an unusual presentation of this infection.
Case Presentation
A 27-year-old male crop surveyor presented with axial proptosis and double vision in the left eye. The diplopia was more pronounced on left lateral gaze and was asso-ciated with blurred vision and occasional watering of the eyes. There was no postural or diurnal variation in the signs and symptoms. The size of the axial proptosis did not vary with straining, thereby ruling out an intracranial connection. The patient’s medical history revealed no comorbidities, prior nasal or ophthalmological surgeries, and no evidence suggestive of an immunocompromised state, such as prolonged corticosteroid use, chemotherapy, haematological malignancy, or organ transplantation.
Clinical examination of the eyes revealed left-sided axial proptosis with normal vision in both eyes. The proptosis in the left eye measured approximately 23 mm from the lateral orbital margin to the apex of the cornea. The finger insinuation test was positive in the left eye. Extraocular movements of the left eye were restricted in all directions.
Diagnostic nasal endoscopy was normal except for mucoid discharge noted in the left middle meatus.
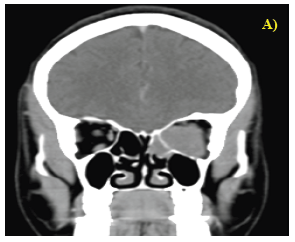
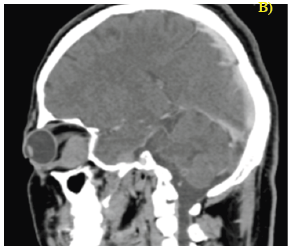
Contrast-enhanced computed tomography (CECT) of the paranasal sinuses (PNS) and orbits revealed a large, well-defined, homogeneously enhancing soft-tissue density lesion involving both the intra and extraconal spaces of the left orbit, extending up to the orbital apex. The left optic nerve was displaced supero laterally by the lesion. Additionally, hypoenhancing lesions were noted in the bilateral sphenoid sinuses and the left posterior ethmoid sinus (Figures 1 & 2).
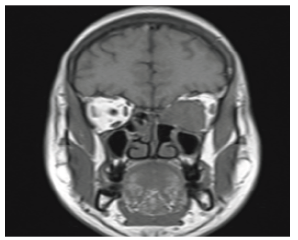
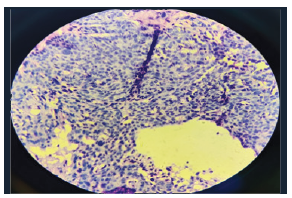
Magnetic resonance imaging (MRI) of the PNS and orbits (Figure 3) demonstrated an ill-defined, fusiform, t2 hypointense lesion with homogeneous enhancement involving the medial rectus muscle, with extensions suggestive of a pseudotumour The patient underwent endoscopic sinus surgery with excision of the intraorbital mass via Denker’s approach under general anaesthesia.3,4 The orbital mass was removed in toto and submitted for histopathological examination, which revealed features consistent with hyalohyphomycosis (Figure 4).
Postoperatively, the patient was started on antifungal therapy with itraconazole, and nasal saline irrigation was done. The patient underwent endoscopic sinus surgery with excision of the intraorbital mass via Denker’s approach under general anaesthesia.3,4 The orbital mass was removed in toto and submitted for histopathological examination, which revealed features consistent with hyalohyphomycosis (Figure 4).
Postoperatively, the patient was started on antifungal therapy with itraconazole, and nasal saline irrigation was done.
Discussion
Hyalohyphomycosis is a rare entity in routine clinical practice. Superficial forms, like onychomycosis and dermatomycosis, are commonly encountered by dermatologists.5 However, deep infections including osteomyelitis and disseminated disease have also been reported.6,7 Subcutaneous variants involving the rhino-orbital region are exceedingly uncommon. We report a case of rhino-orbital hyalohyphomycosis involving the paranasal sinuses and orbit in an immunocompetent, middle-aged male. The diagnosis was established by histopathological examination. The hypodense mass identified on imaging was successfully managed through endoscopic sinus surgery and excision of the intraorbital mass via Denker's approach under general anaesthesia. Histopathological analysis confirmed the diagnosis of hyalohyphomycosis.
Postoperatively, the patient was treated with itraconazole and advised regular nasal saline irrigation, consistent with regimens reported effective in previous cases.8 Recurrence of hyalohyphomycosis in immunocompetent individuals, especially with Purpureocillium lilacinum species, has been documented.9 In this case, regular follow-up with diagnostic nasal endoscopy revealed no evidence of recurrence to date.
Rhino-orbital hyalohyphomycosis should be considered in the differential diagnosis of unilateral intra-orbital mass or proptosis, even in immunocompetent individuals. Early recognition and prompt management are essential to prevent dissemination of the fungal infection and to reduce the risk of morbidity and mortality.
Conflict of Interest
None
Supporting File
References
1. Hospenthal DR. Hyalohyphomycosis: Infec-tion due to hyaline moulds. In: Diagnosis and treatment of fungal infections [Internet]. Springer, Cham; 2015 [cited 2024 Nov 19]. p. 141-9. Available from: https://link.springer.com/ chapter/10.1007/978-3-319-13090-3_11
2. Nucci M, Anaissie E. Emerging fungi. Infect Dis Clin North Am 2006; 20(3):563-79.
3. Lee JT, Chiu AG. Endoscopic Denker approach for anterior maxilla tumors. In: Atlas of endoscopic sinus and skull base surgery [Internet]. Elsevier; 2019 [cited 2024 Nov 19]. p. 183-190.e1. Available from: https://linkinghub.elsevier.com/retrieve/pii/ B9780323476645000225
4. Ahilasamy N, Narendrakumar V, Kumar RD, et al. How I do it:- Endoscopic Reverse Denker’s Approach. Indian J Otolaryngol Head Neck Surg 2023;75(Suppl 1):781-784.
5. Mochizuki T, Tsuboi R, Iozumi K, et al. Guide-lines for the management of dermatomycosis (2019). J Dermatol 2020;47(12):1343-1373.
6. Ramakrishna JM, Libertin CR, Sherman CE, et al. Tibial osteomyelitis: A case report of hyalohy-phomycosis. Acta Sci Orthop 2020;3(3):01-4.
7. Hasan N. Human hyalohyphomycoses: A review of human infections due to Acremonium spp., Paecilomyces spp., Penicillium spp., Talaromy-ces spp., and Scopulariopsis spp. In: Ghannoum MA, Perfect JR, editors. Antifungal Therapy [Internet]. 2nd ed. Second edition. | New York, NY: CRC Press, [2019]: CRC Press; 2019 [cited 2024 Nov 19]. p. 325-35. Available from: https://www. taylorfrancis.com/books/9780429687709/cha-pters/10.1201/9780429402012-20
8. Konda D, Balasubramanian P, Mohanan S, et al. Hyalohyphomycosis (Fusariosis): Atypical presentation in an immunocompetent individual responding to itraconazole. Indian Dermatol Online J 2024;15(2):263-5.
9. McGeachie DL, Boyce AE, Miller RM. Recurrent cutaneous hyalohyphomycosis secondary to Purpureocillium lilacinum in an immunocompetent individual. Australas J Dermatol 2021;62(3):e411-e413.