RGUHS Nat. J. Pub. Heal. Sci Vol: 15 Issue: 4 eISSN: pISSN
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Amulya Aggarwal, Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India.
2Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India
3Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India
4Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India
5Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India
6Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India
*Corresponding Author:
Amulya Aggarwal, Department of Urology, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India., Email: dramulyaaggarwal90@gmail.com
Abstract
Eosinophilic cystitis (EC) is a rare inflammatory condition of the urinary bladder characterized by a predominant infiltration of eosinophils into the bladder wall. About 200 cases of eosinophilic cystitis have been reported till date. The pathogenesis of EC remains uncertain, but it is often linked to allergic reactions, parasitic infections, and certain medications. The three patients described in this series presented with lower urinary tract symptoms (LUTS) and hematuria. Diagnosis was ascertained by cystoscopy and tissue biopsy. In all three cases, the lesion was completely excised and submitted for histopathological examination. All three patients received oral antihistamines for three weeks, and one patient received oral prednisolone. None of the patients showed recurrence during follow-up. A combination of imaging studies, urinalysis, and histopathological biopsy can effectively confirm the condition. In our case series, early diagnosis and appropriate treatment led to favorable outcomes.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Eosinophilic cystitis (EC) is a rare inflammatory condition of the urinary bladder characterized by a predominant infiltration of eosinophils into the bladder wall. First described over 85 years ago, EC has been associated with various etiological factors, including food allergens, infections, medications, and other genitourinary conditions.1
Clinically, EC presents with nonspecific urinary symptoms such as dysuria, haematuria, frequency, and urgency. Notably, in adults, it can manifest as a bladder mass that clinically and radiographically mimics invasive bladder cancer. This resemblance often leads to misdiagnosis and poses significant challenges in clinical management.2
The pathogenesis of EC remains uncertain, but it is often linked to allergic reactions, parasitic infections, and certain medications. Histologically, EC is characterized by an intense eosinophilic infiltrate in the acute phase and fibrosis in the chronic phase.1
Given its rarity and the potential for misdiagnosis, especially when EC presents as a mass-like lesion, it is crucial for clinicians to consider it in the differential diagnosis of bladder masses to avoid unnecessary radical surgical interventions.2
This case series aims to shed light on cases of EC that clinically and radiographically mimic bladder cancer, emphasizing the importance of accurate diagnosis and appropriate management strategies.
Case Presentation
Case 1
A 64-year-old male presented to our department with complaints of poor urinary stream, frequency, and dysuria. He had no known medical comorbidities. Urinalysis revealed pyuria, microscopic haematuria and positive nitrites. He was initially started with antibiotics and ultrasonography was ordered, which revealed focal, polypoidal, irregular wall thickening of the anterior wall of bladder with prostatomegaly and median lobe hypertrophy (Figure 1).
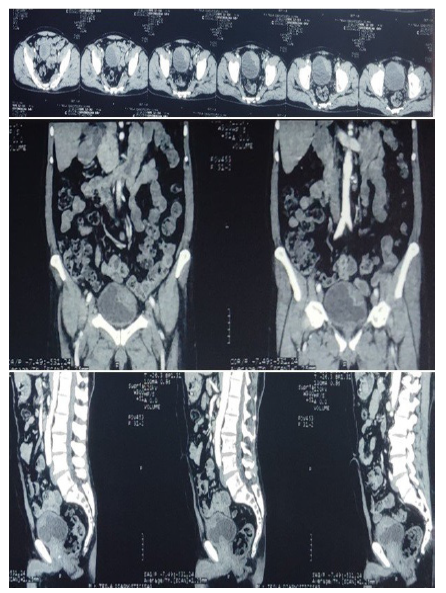
Contrast enhanced CT scan of KUB region revealed an irregular, heterogeneously enhancing lesion measuring 5.2 X 4.8 X 2.5 cm, arising from the anterior and left lateral walls of the urinary bladder. The differential diagnosis included carcinoma of the bladder (Figure 2).
Cystoscopy revealed a vulnerable, erythematous bladder mucosa and a bladder mass. The mass was resected using bipolar cautery, and biopsies of the bladder mucosa were obtained along with a transurethral resection of the prostate. Histological examination showed dense eosinophilic infiltration (>20 eosinophils per five high-power fields), granulation tissue, and fibrosis. The patient’s symptoms resolved following surgery. Treatment with prednisone was not considered and the patient was prescribed tablet levocetrizine for three weeks.
Case 2
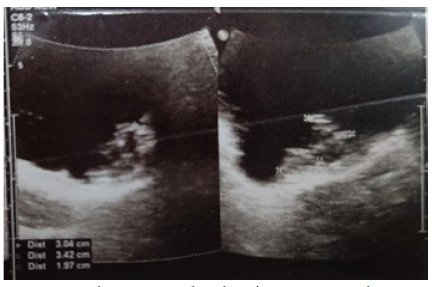
A 55-years-old female was admitted to our department with complaints of frequency, urgency, and nocturia. She had no significant medical history. Urinalysis revealed microscopic haematuria. Ultrasonography showed a 4 mm polyp in the urinary bladder near the left vesicoureteric junction (VUJ) and increased bladder wall thickness (Figure 3).
A contrast enhanced CT scan of the KUB region revea-led a 4 mm polyp arising from the bladder base near the left vesicoureteric junction, with normal upper urinary tracts. Cystoscopy confirmed these findings, and a transurethral resection of the polyp was performed. Histological examination revealed subepithelial infiltration of inflammatory cells, predominantly eosinophils. Postoperatively, the patient was started on oral antibiotics for two weeks and remained asymptomatic at nine months of follow-up. Treatment with prednisone was not considered.
Case 3
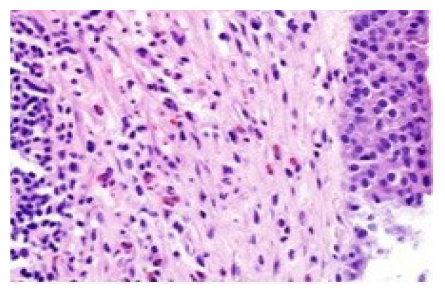
A 56-year-old man was referred to our department with gross haematuria, frequency, urgency, and dysuria for over one month. His medical history was significant for hypertension. Urinalysis revealed pyuria, haematuria, and proteinuria. He had been treated for a suspected urinary tract infection three weeks earlier at another facility; subsequent urine culture was negative. CT scan revealed thickened bladder wall with normal upper urinary tracts. Cystoscopy done prior to random biopsies revealed edematous, hyperemic bladder mucosa, raising suspicion for carcinoma in situ. Histopathological examination of the biopsies showed benign lymphoid follicles with eosinophilia infiltration (Figure 4).
He was treated with prednisone 37.5 mg per day for 10 days. Haematuria subsided and the frequency at daytime improved; however, the patient continued to experience frequent urination at night.
Discussion
Unlike other forms of cystitis, eosinophilic cystitis (EC) is a rare inflammatory condition with a low incidence rate. While the exact number varies slightly across reports, approximately 200 cases have been documented in the medical literature.3 Among 135 reported cases, patient ages ranged from 5 to 87 years, with a mean age of 41.6 years, and no significant gender predisposition.4 EC has been linked to the BRAFI463T gene mutation, which may result in molecular abnormalities in hematopoietic stem cells or myeloid cells.5 The pathogenesis of EC involves an anaphylactic response triggered by various physical, chemical, biological, or pathological factors; however, in approximately one-third of cases, the exact cause remains unidentified.4 Potential triggers include parasites, dust, bladder trauma, and hypersensitivity to food or medications. These antigens may elicit an immunoglobulin E-mediated response, leading to the release of eosinophilic chemotactic factors, and subsequent damage through the release of lysosomal enzymes and cytokines.6
Peripheral eosinophilia is detected in about 43% of cases; however, more than half of patients do not exhibit a significant elevation in eosinophil levels.7 Due to the rapid degradation of eosinophils in urine, urinalysis findings typically include proteinuria, microscopic haematuria, and pyuria, while eosinophiluria is observed only in rare cases.8 The most common symptoms of EC include bladder irritation, with frequency reported in 67% of cases and dysuria in 62%. Imaging studies do not provide definitive diagnostic features, as EC may present with diffuse or irregular bladder wall thickening, nodular formations, or large masses. The condition lacks characteristic imaging findings, and reports describe tumour-like lesions, polyps, follicles, ulcers, mucosal edema, hyperaemia, and erythema. Smaller tumour-like masses, such as in our case, are relatively uncommon and can lead to misdiagnosis. Ultimately, histopathological evaluation is required for diagnosis, with EC confirmed by the presence of more than 25 eosinophils per high-power field.9 In the acute stage, significant eosinophilic infiltration of the mucosa and submucosa is observed, whereas chronic EC presents with persistent mucosal inflammation without prominent eosinophilia.10 This may explain why cystoscopic biopsy in our patient revealed chronic mucosal inflammation without eosinophilic infiltration. Reports on EC occurring alongside other diseases are limited.
For patients presenting with tumour-like lesions, we hypothesize that EC and cystitis glandularis (CG) may exacerbate each other’s progression, though it remains unclear whether EC predisposes individuals to CG or malignancy. There is no established consensus on EC management; initial treatment typically includes glucocorticoids, antihistamines, and antibiotics.11 The recurrence rate among patients treated medically is approximately 17%, while it drops to 2.6% following surgical intervention.7 In our cases, diagnostic transurethral resection of the bladder was performed, followed by treatment with antibiotics, glucocorticoids (in one patient), and antihistamines.
Due to the rarity of EC, standardized treatment protocols have not been established. Some cases follow an unpredictable course, and medical therapy is often administered at different disease stages. Occasionally, EC remains asymptomatic and is incidentally diagnosed during cystoscopic evaluation for a history of bladder cancer.11 In some instances, symptoms resolve upon removal of the triggering factor. Surgery is generally recommended for cases involving large tumour-like or follicular lesions.12 Our patient recovered uneventfully without recurrence, suggesting that surgical management is preferable in cases of large, tumour-like EC coexisting with other pathologies such as cystitis glandularis. In conclusion, large tumor-like eosinophilic cystitis associated with cystitis glandularis is rare, and malignancy must be ruled out. We believe that an early biopsy led to an accurate diagnosis, and timely intervention contributed to a favourable prognosis.
Eosinophilic cystitis is an uncommon inflammatory condition of the bladder, characterized by eosinophilic infiltration of the bladder wall. Its symptoms often mimic those of bladder tumours, making diagnosis challenging. However, a combination of imaging studies, urinalysis, and histopathological biopsy can effectively confirm the condition. In most cases, early diagnosis and appropriate treatment lead to favorable outcomes.
Declarations
Ethics approval and consent to participate
Ethics approval was not required by the authors’ institution, as the present study is a case series. All methods were performed in accordance with the relevant guidelines and regulations. Informed signed consent to participate was obtained from the patients.
Conflict of Interest
None
Funding Declaration
The study is self-funded.
Consent for Publication
Informed written consent has been taken from all three patients regarding publication of their scan images and others.
Supporting File
References
1. Cai T, Verze P, Malossini G, et al. The spectrum of eosinophilic cystitis in males: A clinical and pathological study of 29 cases. Arch Pathol Lab Med 2009;133(2):289-294.
2. Cleva M, Bruschi E, Bruschi F, et al. Eosinophilic cystitis: A case report of a pseudotumoral lesion. J Ultrasound 2023;26(4):935-937.
3. Ye JB, Chen Q, Zeng K, et al. Eosinophilic cystitis complicated with cystitis glandularis: a case report. BMC Urol 2022;22:1-4.
4. Li G, Cai B, Song H, et al. Clinical and radiological character of eosinophilic cystitis. Int J Clin Exp Med 2015;8(1):533-9.
5. Choi MY, Tsigelny IF, Boichard A, et al. BRAF mutation as a novel driver of eosinophilic cystitis. Cancer Biol Ther 2017;18(9):655-9.
6. Galutira PJT, Canonigo BB, Cabansag MRF, et al. Presenting manifestations of eosinophilic cystitis in two Filipino children. Int Urol Nephrol 2010;42(3):557-63.
7. van den Ouden D. Diagnosis and management of eosinophilic cystitis: a pooled analysis of 135 cases. Eur Urol 2000;37(4):386-94.
8. Kumar S, Sharma V, Ganesamoni R, et al. Eosinophilic cystitis mimicking tuberculosis: an analysis of five cases with review of literature. Urol Ann 2013;5(1): 50-2.
9. Zhou AG, Amin A, Yates JK, et al. Mass forming eosinophilic cystitis in pediatric patients. Urology 2017;101:139-41.
10. Kim MS, Park H, Park CS, et al. Eosinophilic cystitis associated with eosinophilicenterocolitis: case reports and review of the literature. Br J Radiol 2010;83(990):e122-5.
11. Werbrouck C, Marrannes J, Verhamme L, et al. Eosinophilic cystitis mimicking bladder tumor. JBR-BTR 2014;97(6):375.
12. Chinese Urology Association. Chinese expert consen-sus on clinical diagnosis and treatment of glandular cystitis. Clin J Urol 2020;41(8):566-8.