RGUHS Nat. J. Pub. Heal. Sci Vol: 15 Issue: 4 eISSN: pISSN
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Department of Anesthesiology, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India
2Department of Anesthesiology, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India
3Department of Anesthesiology, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India
4Dr. Mohsina Yasmeen, Assistant Professor, Department of Anesthesiology, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India.
*Corresponding Author:
Dr. Mohsina Yasmeen, Assistant Professor, Department of Anesthesiology, Bangalore Medical College and Research Institute, Bangalore, Karnataka, India., Email: drmohsinayasmeen@gmail.com
Abstract
Background: Evidence suggests that gas insufflation during laparoscopic surgery may compromise diaphragmatic function, potentially leading to postoperative respiratory challenges. The intraoperative use of positive end-expiratory pressure (PEEP) and pulmonary recruitment maneuvers could prevent atelectasis, reducing respiratory complications. This study examined the effect of PEEP and recruitment maneuvers on diaphragmatic activity during laparoscopic procedures.
Methods: This randomized study involved patients undergoing laparoscopic abdominal surgery, categorized into three groups via computer-generated selection: Group A (zero PEEP), Group B (PEEP at 5 cmH2O), and Group C (PEEP plus recruitment maneuvers). Measurements included diaphragmatic excursion, peak inspiratory pressure, hemodynamic parameters (HR, MAP), and lung compliance.
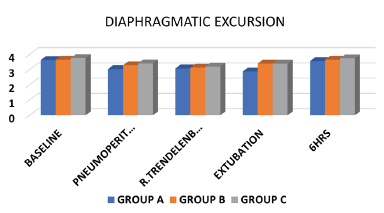
Results: Average diaphragmatic excursion (in cm) was measured at several stages: baseline, pneumoperitoneum, reverse Trendelenburg, after extubation, and at six hours postoperatively. In Group A, values were recorded as 3.63±0.28, 3.04±0.18, 3.08±0.008, 2.88±0.34, and 3.56±0.33, respectively. Group B values were 3.65±0.27, 3.29±0.30, 3.13±0.29, 3.40±0.37, and 3.65±0.29, while Group C values were 3.75±0.31, 3.41±0.28, 3.20±0.30, 3.40±0.34, and 3.74±0.31. Notably, Group A had significantly reduced compliance compared to Groups B and C, while values in Group C were consistently higher, despite no statistical difference between B and C.
Conclusion: The use of PEEP during laparoscopic surgeries supports diaphragmatic excursion. Furthermore, recruitment maneuvers enhance diaphragmatic movement and dynamic compliance, albeit with elevated peak inspiratory pressures compared to the other groups
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Laparoscopic procedures are among the most commonly performed surgeries globally. They typically involve CO₂ insufflation into the abdominal cavity, which increases intra-abdominal pressure. This rise in pressure can lead to several respiratory changes, such as decreased functional residual and vital capacities formation of atelectasis in the dependent lung regions, and reduced respiratory compliance. Postoperative atelectasis significantly affects gas exchange and is a primary cause of hypoxia following surgery.1 Protective ventilation strategies, such as PEEP (Positive End- Expiratory Pressure) and pulmonary recruitment maneuvers, have been shown to reduce postoperative pulmonary complications.2 Research has suggested that gas insufflation during laparoscopic surgery may impair diaphragmatic function by increasing resistance and limiting diaphragm movement, thereby reducing lung volumes.3-8 Previous studies have linked impaired diaphragmatic function after abdominal surgery with the onset of postoperative pulmonary dysfunction.9-19 Ultrasound has emerged as a non-invasive, effective tool for evaluating diaphragmatic function, including assessing diaphragm thickness and excursion. This technique provides high-resolution, real-time imaging that is accessible and reliable in the operating theater.20-23 The goal of this study was to evaluate the effects of PEEP and recruitment maneuvers on diaphragmatic excursion during pneumoperitoneum in laparoscopic surgeries.
Materials and Methods
This prospective, randomized clinical trial involved 63 patients undergoing laparoscopic abdominal surgeries at Bangalore Medical College and Research Institute from March to November 2021. Ethical clearance was obtained before the study (CTRI/2022/02/039942). Patients eligible for inclusion were those with a breath-holding time greater than 40 seconds and classified as ASA I or II, undergoing laparoscopic cholecystectomy. Exclusion criteria included patients with severe systemic illnesses, respiratory disorders, diaphragmatic diseases, BMI over 30, or those undergoing complex or recurrent abdominal surgeries, as well as patients whose surgeries were converted to open procedures. The primary objective was to assess diaphragmatic excursion and respiratory mechanics, such as peak inspiratory pressure (PIP) and lung compliance. Secondary objectives included evaluating hemodynamic parameters, including heart rate (HR), mean arterial pressure (MAP), and end-tidal CO₂ (ETCO₂). Participants were randomly assigned to one of three groups: Group A (no PEEP), Group B (PEEP at 5 cm H₂O), and Group C (PEEP at 5 cm H₂O with recruitment maneuvers). The study was conducted blindly, with anaesthesia management handled by anaesthesiologists who were not involved in data collection or analysis.
Before surgery, baseline parameters such as breath-holding time and ultrasound-guided diaphragmatic excursion were recorded. Alprazolam 0.5 mg was given the night before surgery. On the day of surgery, after transfer to the preoperative room, pulse oximeter, non-invasive blood pressure, and ECG monitors were connected and baseline parameters were recorded. An intravenous line with 18G IV cannula was obtained and an IV infusion of 500 mL Ringer’s lactate was initiated. General anaesthesia was induced using intravenous midazolam, fentanyl, propofol, and vecuronium. Endotracheal intubation was performed with an appropriate-sized cuffed tube. Anaesthesia was maintained with O2, air, and isoflurane. Initial flow was set at 4 L/min until equilibrium between inspired and end-tidal isoflurane concentrations was achieved, after which it was reduced to 2 L/min. Mechanical ventilation was volume-controlled, with a tidal volume of 6-8 mL/ kg, respiratory rate of 12-14 breaths per minute, and an inspired oxygen fraction of 50%, to maintain ETCO₂ between 35 to 45 mmHg. Inhaled concentrations of isoflurane were set to maintain a minimum alveolar concentration (MAC) of 0.8-1. Inj. paracetamol 1 mg IV was administered intraoperatively for analgesia. Patients allocated to Group A received mechanical ventilation without PEEP, Group B received ventilation with 5 cm H₂O of PEEP, and Group C received 5 cm H₂O of PEEP combined with intermittent recruitment maneu-vers. These maneuvers involved maintaining an airway pressure of 30 cm H₂O for 30 seconds at critical proce-dural stages (post-induction, after pneumoperitoneum, after patient repositioning, and after CO₂ exsufflation). Respiratory mechanics, including ETCO2, peak airway pressure, lung compliance, diaphragmatic excursion, along with hemodynamic parameters like heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), peripheral oxygen saturation (SpO2), and fraction of inspired air (FIO2) were measured at the following time points: post-induction of anaesthesia, 5 minutes after completion of pneumoperitoneum, 5 minutes after patient repositioning, every 15 minutes thereafter until the end of surgery, and finally after exsufflation of pneumoperitoneum. Isoflurane administration was discontinued 10 minutes before the end of surgery. At the conclusion of the procedure, the patient was reversed with Inj. neostigmine 0.05 mg/kg and Inj. glycopyrrolate 0.01 mg/kg. Patients were extubated after surgery and shifted to the recovery area. Postoperative assessments of diaphragmatic excursion and peak expiratory flowrate were conducted at 6 and 24 hours using a 5-10 MHz ultrasound probe. Diaphragmatic thickness and mobility were measured during the end-expiratory phase, and excursion was evaluated by observing craniocaudal displacement in M-mode. Changes in diaphragmatic thickness were expressed as a percentage, with 20% considered the lower limit value.
The diaphragmatic excursion was measured using a GE Healthcare Module - LOGIQ E10, equipped with a straight-array probe operating at 5-10 MHz. The probe was placed in the right subcostal plane, midway between the right anterior axillary and midclavicular lines, with the liver serving as an acoustic window. Using M-mode ultrasound, diaphragmatic mobility was assessed by measuring the craniocaudal displacement of the hypoechoic diaphragm between two echogenic lines (pleura and peritoneum). Gain and depth settings were optimized for diaphragm visualization, and the focus was set at the diaphragm level. Measurements were taken during forced inspiration with patients in the supine position. Three readings were obtained per patient, and the mean value was used for analysis. The technique was validated against gold-standard methods in previous studies, with normal upper limits for diaphragmatic excursion defined as 4.7 cm for men and 3.7 cm for women. Inter and intra-observer variability was assessed, yielding an intraclass correlation coefficient of 0.95. Normal diaphragmatic thickness ranges from 0.17 - 0.20 cm in men and 0.13 - 0.15 cm in women.
Complications, including barotrauma parameters such as pneumothorax, surgical emphysema, and reduced air entry, were also recorded.
Sample size
The sample size was calculated based on the parameter diaphragmatic excursion for three groups: Group A (no PEEP), Group B (PEEP 5) and Group C (pulmonary recruitment maneuver), following the study by Doa Abou et al.2 The sample size calculation used the formula: n=2(Zα+Z1-β) 2 σ 2 /d2, Where Zα=standard table value for 95%CI=1.96, Z1-β=standard table value for 80% power=0.95, Σ=standard deviation=3.72, d=effect size=0.6095. Substituting the values: N = 2(1.96+0.95)2×(3.72)2 /(0.6095)2; n=21 per group. Thus, the total sample size required was 63 participants.
Results
The demographic profile of the study participants, including age, weight, gender, ASA grade, and surgery duration, was similar across the three groups. The study included 63 patients, comprising 33 females and 30 males. The mean age was 43.85 ± 10.04 years in Group A, 43.06 ± 12.40 years in Group B, and 43.77 ± 10.10 years in Group C (Table 1).
Statistical analysis revealed a significant difference in diaphragmatic excursion between the control group (Group A) and the intervention groups (Group B and Group C). There was no significant difference in diaphragmatic excursion between Group B (PEEP only) and Group C (PEEP with recruitment maneuvers). The mean diaphragmatic excursion at different stages of the procedure was significantly lower in Group A compared to the other two groups (P value 0.743, 0.742, 0.000, 0.000, 0.000] (Figure 1).
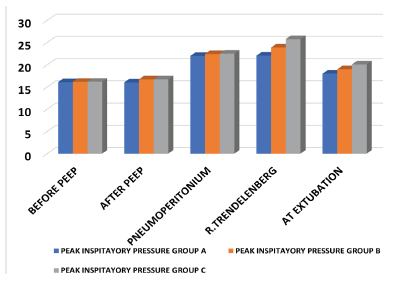
Peak inspiratory pressure (PIP) values were significantly higher after pneumoperitoneum and reverse Trendelenburg positioning in all groups, though there were no significant differences in PIP across the groups [P value 0.236, <0.001, <0.001, 0.001] (Figure 2). Dynamic compliance was significantly lower in Group A at all time points compared to Groups B and C, with Group C exhibiting higher compliance throughout the procedure (Table 2).
The heart rate (HR) and mean arterial pressure (MAP) were compared with the baseline values across three groups (Table 3, Figure 3). No complications were observed in association with PEEP or the pulmonary recruitment maneuver.
A statistically significant difference was observed at the time of pneumoperitoneum and 15 minutes thereafter, with a P value <0.005*.
A statistically significant difference was observed in Groups 2 and 3 compared with Group 1 (P-value <0.001).
Discussion
The results of this study emphasize the importance of protective ventilation strategies in preserving diaphragmatic function during laparoscopic surgery. The use of pulmonary recruitment maneuvers, along with PEEP, was associated with better lung mechanics, reflected in improved dynamic compliance and reduced risk of postoperative pulmonary complications. These findings align with previous studies that highlight the efficacy of PEEP and recruitment maneuvers in maintaining diaphragmatic excursion and optimizing respiratory outcomes during surgery.24-26
In the study conducted by Doa et al., excursion of the diaphragm decreased in the three groups and was significantly lower in the group with PEEP 0 compared to groups with PEEP 5 and PEEP 10 after pneumoperitoneum up to two hours after initiation of the head-down position. Peak inspiratory pressure was significantly higher in groups with PEEP 10 compared to groups with PEEP 5 and 0.2 The application of PEEP helps preserve diaphragmatic excursion and significantly reduces the incidence of atelectasis. In the study conducted by Sheren et al., diaphragmatic excursion (DE) did not differ significantly among the three groups before induction of anaesthesia.27 However, after pneumoperitoneum and throughout the procedure up to 24 hours postoperatively, a statistically significant difference was observed between the control group and the two intervention groups (PEEP 5 and PEEP with RM), with the control group showing a significant decrease in DE.
In line with earlier studies, the combination of PEEP and recruitment maneuvers did not show additional benefits over PEEP alone, suggesting that PEEP plays a central role in mitigating the adverse effects of pneumoperitoneum on diaphragmatic excursion. This indicates that PEEP alone may be sufficient for preserving diaphragmatic function, while the addition of recruitment maneuvers might not offer further advantages.
Ultrasound-guided ventilation strategies provide real-time monitoring of diaphragmatic function, allowing for more tailored and effective respiratory management during surgery. The integration of ultrasound to guide recruitment maneuvers for atelectasis is an area of growing interest, offering the potential for improving perioperative respiratory management.28
Further research is warranted to elucidate the optimal timing and frequency of pulmonary recruitment maneuvers during laparoscopic surgery, as well as their long-term impact on postoperative outcomes. Additionally, prospective studies incorporating larger patient cohorts and longer follow-up periods are needed to validate the efficacy of ultrasound-guided ventilation strategies in diverse surgical populations. By advancing our understanding of perioperative respiratory management, we can continue to enhance patient care and optimize surgical outcomes in the era of minimally invasive surgery.
Conclusion
PEEP helps preserve diaphragmatic excursion during laparoscopic surgery. Pulmonary recruitment maneuvers enhance diaphragmatic excursion and dynamic compliance, although they are associated with a rise in peak inspiratory pressure. By incorporating these strategies, guided by ultrasound, clinicians can optimize perioperative respiratory care and reduce the risk of postoperative pulmonary complications. These findings underscore the significance of personalized ventilation strategies in minimizing pulmonary complications during minimally invasive surgeries.
Conflict of Interest
Nil
Supporting File
References
1. Hurley RW, Murphy JD, Wu CL. Acute postopera-tive pain. In: Miller RD, editor. Miller’s anaesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015.p. 2974-81.
2. Rashwan DAE, Mahmoud HE, Nofal WH, et al. Ultrasonographic evaluation of the effect of positive end-expiratory pressure on diaphragmatic functions in patients undergoing laparoscopic colorectal surgery: A prospective randomized comparative study. J Anesth Clin Res 2018;9:843.
3. Johannsen G, Andersen M, Juhl B. The effect of general anesthesia on the hemodynamic events during laparoscopy with CO-insufflation. Acta Anaesthesiol Scand 1989;33:132-6.
4. Suh MK, Seong KW, Jung SH, et al. The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol 2010;59:329-34.
5. Midgley S, Tolley DA. Anaesthesia for laparoscopic surgery in urology. Euro Assoc Urol 2006;4:241-5.
6. O’Malley C, Cunningham AJ. Physiologic changes during laparoscopy. Anesthesiol Clin North America 2001;19:1-19.
7. Kalmar AF, Foubert L, Hendrickx JF, et al. Influence of steep Trendelenburg position and CO (2) pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth 2010;104: 433-9.
8. El-Dawlatly AA, Al-Dohayan A, Abdel-Meguid ME, et al. The effects of pneumoperitoneum on respiratory mechanics during general anesthesia for bariatric surgery. Obes Surg 2004;14:212-5.
9. Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 2009;111: 979-87.
10. Brescia A, Tomassini F, Berardi G, et al. Development of an enhanced recovery Dіer surgery (ERAS) protocol in laparoscopic colorectal surgery: results of the first 120 consecutive cases from a university hospital. Updates Surg 2017;69:359-365.
11. Valenza F, Chevallard G, Fossali T, et al. Managementof mechanical ventilation during laparoscopic surgery. Best Pract Res Clin Anaesthesiol 2010;24:227-41.
12. Restrepo RD, Braverman J. Current challenges in the recognition, prevention, and treatment of perioperative pulmonary atelectasis. Expert Rev Respir Med 2015;9(1):97-107.
13. Gunnarsson L, Strandberg A, Brismar B, et al. Atelectasis and gas exchange impairment during enflurane/nitrous oxide anaesthesia. Acta Anaesthesiol Scand 1989;33:629-637.
14. Brismar B, Hedenstierna G, Lundquist H, et al. Pulmonary densities during anesthesia with muscular relaxation a proposal of atelectasis. Anesthesiology 1985;62:422-8.
15. Coppola S, Froio S, Chiumello D. Protective lung ventilation during general anesthesia: is there any evidence? Crit Care 2014;18(22): 210.
16. Jo YY, Lee JY, Lee MG, et al. Effects of high positive end-expiratory pressure on hemodynamics and cerebral oxygenation during pneumoperitoneum in the Trendelenburg position. Anaesthesia 2013;68:938-43.
17. Suh MK, Seong KW, Jung SH, et al. The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol 2010;59:329-34.
18. Strang CM, Hachenberg T, Fredén F, et al. Development of atelectasis and arterial to end-tidal PCO2-difference in a porcine model of pneumoperitoneum. Br J Anaesth 2009;103: 298-303.
19. Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg 2009;109:1511-6.
20. Yu X, Zhai Z, Zhao Y, et al. Performance of lung ultrasound in detecting peri-operative atelectasis after general anesthesia. Ultrasound Med Biol 2016;42(12):2775-2784.
21. Le Neindre A, Mongodi S, Philippart F, et al. Thoracic ultrasound: potential new tool for physiotherapists in respiratory management. A narrative review. J Crit Care 2016;31(1):101-9.
22. Monastesse A, Girard F, Massicotte N, et al. Lung ultrasonography for the assessment of perioperative atelectasis: a pilot feasibility study. Anesth Analg 2017;124(2):494-504.
23. Acosta CM, Maidana GA, Jacovitti D, et al. Accuracy of transthoracic lung ultrasound for diagnosing anesthesia-induced atelectasis in children. Anesthesiology 2014;120(6):1370-9.
24. Bluth T, Neto AS, Schultz MJ, et al. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA 2019;321(23):2292-305.
25. Sen O, Doventas YE. Effects of different levels of end-expiratory pressure on hemodynamic, respiratory mechanics and systemic stress response during laparoscopic cholecystectomy. Braz J Anesthesiol 2017;67(1):28-34.
26. Whalen FX, Gajic O, Thompson GB, et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth Analg 2006;102(1):298-305.
27. Abd Ellatif SE, Mowafy SMS. Ultrasonographic evaluation of the effect of recruitment maneuvers and positive end-expiratory pressure on diaphragmatic functions in obese patients undergoing laparoscopic sleeve gastrectomy: A randomized controlled study, Egypt J Anaesth 2020;36(1):69-77.
28. Tusman G, Acosta CM, Costantini M. Ultrasono-graphy for the assessment of lung recruitment maneuvers. Crit Ultrasound J 2016;8(1):8.